Colon Cancer Specialist Mumbai
Colorectal cancer – commonly known as colon cancer, or bowel cancer – is any cancer that affects the last section of the digestive system. This usually means the colon (large bowel) or rectum (back passage).
Colon cancer is caused by the abnormal growth of cells in the lining of the bowel. Usually small lumps called polyps begin to form. Commonly these lumps are referred to as tumours.
The growth of polyps can be harmless, these are known as benign tumours. However, these polyps can also be caused by the growth of cancer cells. These are called malignant tumours.
If left untreated, these cancerous growths can spread to other parts of the body.
Who Is Affected By Colon Cancer?
Colon cancer affects men and women equally. However, it is the third most common type of cancer in men and the second most common type in women.
Colon cancer usually affects people over the age of 40, with the majority of people who are diagnosed with the condition being over 60 years of age.
Symptoms
The symptoms of colon cancer are similar to those of haemorrhoids (piles), or irritable bowel syndrome (IBS). You might experience:
- Blood in your stools, particularly if the blood appears dark in colour
- Mucus in your stools
- Changes in your bowel movements for example, you may have constipation, or diarrhoea, and
- Abdominal pain or discomfort your abdomen may feel swollen and sore, and you may experience unexplained loss of weight.
You should visit your GP if you begin to display any of the above symptoms.
As the tumour grows, the above symptoms may worsen. Also, in rare cases, you may begin to feel tired, or breathless, for no obvious reason. This may be due to the fact you are having microscopic bleeding (very light or minor bleeding) from your bowel. This can result in anaemia; a condition where the number of red blood cells is reduced so that less oxygen can be carried to the body’s organs and tissues.
Malignant tumours (cancerous cells) often develop to an advanced stage before symptoms start to occur. It is therefore important to note any changes to your stools (faeces).
Cancerous cells that develop around the wall of your bowel can obstruct your stools. This may make them appear more narrowed (almost flattened) in shape. Speak with your GP is you have any concerns.
Causes
The exact cause of colon cancer is unknown.
Polyps
The majority of colon cancers develop within polyps (also known as adenoma). These are often found inside the bowel wall. Polyps can be either:
- Benign lumps that are harmless, or
- Malignant tumours that are cancerous
Age
Age is one of the main factors that is thought to be linked to colon cancer. It appears that your risk of colon cancer increases as you get older, with 85% of people diagnosed with the condition being over the age of 60.
Family History
Genetics also seem to play a significant role in increasing your risk of developing colon cancer. If there is a history of colon cancer in your family, you should speak with your GP about it, as the condition can be passed down to you (inherited) from a member of your family.
If you have a family history of colon cancer, your GP may recommend having the rest of your family screened in order to determine whether they are at increased risk.
Diet
There has been evidence to suggest that if your diet is high in animal protein (meat) and fats, and low in fibre, you are more likely to develop colon cancer. This is because this type of diet is associated with irregular bowel movements. Eating a high fibre diet can reduce your risk of developing colon cancer because it will encourage regular bowel movements.
Lifestyle Factors
Lifestyle factors can also increase your risk of developing colon cancer. These include being overweight, taking very little exercise, and smoking.
Medical Conditions
Colon cancer may also develop as a result of certain medical conditions. For example, if you have inflammatory bowel disease (inflammation of the intestines) or Crohn’s disease (inflammation of the gut), your risk of getting colon cancer will be increased.
Diagnosis
If you have symptoms similar to those of colon cancer (see ‘symptoms section’), your GP will ask you about your symptoms, and may decide to examine you.
Surgical Examination
Most colon cancers can be felt under examination by the colorectal surgeon Using lubricated gloves he/she will conduct a rectal examination. If a malignant tumour (cancerous growth) is lower down your colon, or in your rectum (back passage), it will be easily felt.
Your surgeon will also be checking to see whether you have any abnormal swelling in your rectum. Even if your doctor does not feel any abnormalities, they may still arrange for further tests and examinations to be carried out.
Bowel cancer screening involves checking your stools for any blood. This can either be confirmed by a faecal occult blood (FOB) test or, alternatively, samples may be taken during an sigmoidoscope, or colonoscope, examination. These are both types of stool test which highlight any invisible traces of blood.
Faecal Occult Blood Test (FOB Test)
A small sample of your faeces (stool) will be tested to check for traces of blood. This test can confirm the presence of blood, but is unable to determine where the blood is coming from, or what the cause is.
It is important to remember that the FOB test cannot diagnose bowel cancer, but rather it indicates whether further examinations need to be conducted.
After having a FOB test, you should receive your results from the laboratory within two weeks. The three result types are outlined below.
- A normal result - means no blood was found in your test sample.
- An unclear result - meaning there may have been a slight indication of blood in your sample. In this case, the test will need to be repeated.
- An abnormal result - this means that there is blood present in your sample and you will be offered a colonoscopy (a procedure where a tube with a light at the end of it is inserted into your anus to check for abnormalities).
Sigmoidoscopy And Colonoscopy
Once it has been established that your stools contain blood, your GP may perform a sigmoidoscopy, or a colonoscopy. Both of these procedures involve looking into your rectum for polyps, or other abnormalities.
A thin lighted tube – sigmoidoscope or colonoscope – is inserted through your anus where polyps, or tissue samples may be taken for further testing (biopsy).
A biopsy is a sample of tissue that is taken from either your colon or rectum. This is then viewed under a microscope to check for signs of cancerous cell growth (abnormal cells).
Your GP may also refer you to a colon specialist who will carry out further tests.
Further Examinations
A specialist may perform a virtual colonoscopy (also known as a CT colonography). This uses X-rays to build up a series of images of your colon. A computer then organises these to create a detailed picture that may reveal the presence of polyps, and anything else that appears unusual on the surface of your colon.
Having an X-ray can also diagnose rectal cancer. A fluid called barium will be placed into your bowel, via your back passage, in order to highlight on an X-ray any abnormalities in tissue growth. This procedure is known as barium enema.
If you are diagnosed with colon cancer, you may need further tests to establish the size and position of the cancer. This is known as ‘staging’ and includes the tests described below.
- A computerised tomography (CT) scan, which is sometimes known as a CAT scan, and is used to display the size and position of the tumour.
- An ultrasound scan of your abdomen to help show if the cancer has spread to another part of your body.
- A magnetic resonance imaging (MRI) scan that is used to give a three dimensional image of your bowel.
Treatment
The type of treatment that you receive for colon cancer will depend of certain factors. These include:
- The size and location of the cancer,
- The stage of development of the cancer - whether the cancer has spread to other parts of your body,
- Whether this is a recurrence of the cancer, and
- Your current overall health.
Your specialist will explain all the treatment options available to you. This is a good opportunity for you to ask any questions that you may have, and also get advice about lifestyle changes that will help your recovery. Your specialist will arrange the treatment that is most suited to your circumstances.
Cancer Stages
Once you are diagnosed with colon cancer your tumor will be ‘staged’. This involves your doctor understanding more about your cancer, including how far cancer has spread or grown in size. This helps them to determine the most appropriate course of treatment.
A staging system called the Duke’s classification is often used for colon cancer. This system is explained below.
- Duke A: the cancer is only in the lining of your colon, or rectum.
- Duke B: the cancer has grown in the muscle layer in the wall of your colon, or rectum.
- Duke C: the cancer has spread to at least one lymph node gland near to your colon, or rectum.
- Duke D: the cancer has spread to other parts of your body, often to your liver, or lungs.
Treatment options for colon cancer include chemotherapy, radiotherapy, and surgery.
Surgery
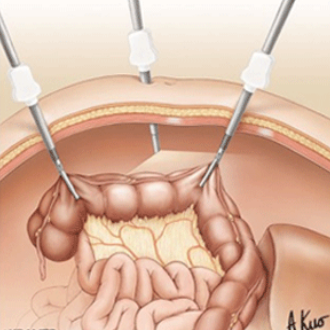
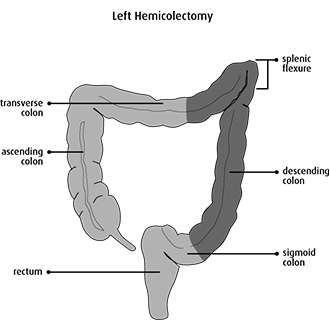
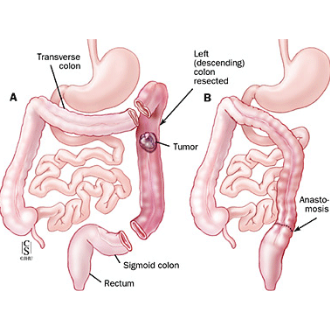
There are many surgical options for treatment of colon cancer.
Surgery is the primary treatment. Whether you require chemotherapy or not will depend on the stage of the disease.
Depending on which side the cancer is the surgery is done accordingly ie that part of the bowel along with the blood supply and the lymphatic drainage is excised
Recovery
Without treatment, polyps (malignant tumours) are likely to increase in size and spread to other parts of your body. The earlier the cancer is treated, the better your chances of being cured.
Your recovery from colon cancer will depend on certain factors:
- The stage your cancer was at when it was diagnosed - whether it was only in the inner lining of your colon, or whether it had spread to other parts of your body,
- Whether the cancer blocked, or created, a hole in your colon,
- Whether the cancer had recurred, and
- The state of your current general health.
Risks
Several factors can increase your risk of developing colon cancer. These are outlined below.
- Your age - if you are over 50 years old you are more likely to develop health problems in your colon.
- Your family history - for example if any members of your family have had colon, rectum or bowel related problems.
- Your own medical history - such as previously having polyps in your colon. If you have also had other conditions, such as inflammatory bowel disease (inflammation of the intestines) or Crohn's disease (inflammation of the gut), this can increase your risk of developing colon cancer.
Prevention
There are several ways that you can help reduce your risk of developing cancer of the colon, rectum, or bowel.
Early Detection
You may decide to have regular screenings for bowel cancer if:
- You have previously had the condition
- You are over 60 years of age,
- You have a close relative who has the condition, or
- You have another condition, such as Crohn's disease (inflammation of the gut)
Diet
Diet plays an important role in preventing the development of colon cancer. You should eat a high-fibre diet with plenty of fruit, vegetables, and carbohydrates (pasta, bread, and rice). This will reduce your risk of getting colon cancer.
You should aim to eat at least five portions of a variety of fruit and vegetables every day. This will help to protect you against many different cancers because of the antioxidant vitamins and minerals they contain.
It is also recommended that you cut down on the amount of processed meat and red meat that you eat. You should limit these to one or two potions a week.
Exercise
Make sure that you exercise regularly. Moderate amounts of exercise are thought to protect you against bowel cancer.
For most people, 30 minutes of exercise, five days a week, should be enough to make you feel the benefits. Ask your GP for advice if you have not exercised before, or for a long time.
Healthy Weight
Try to maintain a healthy weight. Changes to your diet and an increase in your physical activities will help to keep your weight under control.