Rectal Prolapse
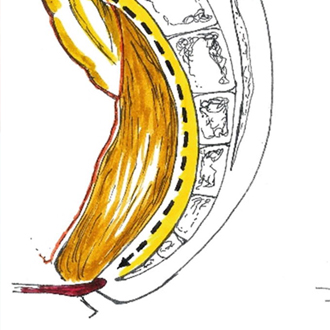
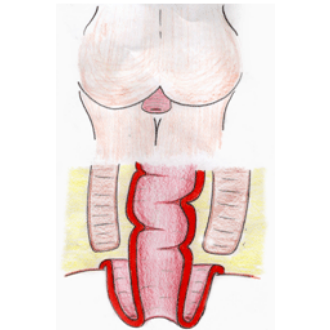
A rectal prolapse occurs when either the lining or indeed the whole of the rectal wall protrudes down to and possibly out through the anus. The rectal wall effectively turns inside out and may appear protruding externally for a variable length outside the anal verge.
What Are The Symptoms Of Rectal Prolapse?
Patients will often notice a bulging from the bowel that comes out with the passage of a bowel motion. In the early stages the prolapse comes down to the anal verge but in more severe cases the prolapse progresses and may be easily felt by the patient externally. Most patients describe the feeling of “something coming or falling out” of the anus that they are able to push back in after a bowel motion. The symptoms are the protrusion of the rectal lining or bowel wall out through the anus. This appears as a reddish mass and may result in some bleeding or mucous being passed. In more severe cases the prolapse continually results in mucous and “dampness” tinged with blood staining the underwear. The prolapse may be very pronounced in some patients and protrude out for several inches. In other cases the prolapse may only appear at the anal verge or indeed be largely internal in nature.
What Is The Cause Of Rectal Prolapse?
There are many different causes of rectal prolapse. They are the result of a general weakness of the supporting ligaments and structures that maintain the rectum and pelvis in normal position. Included in the list of causes of rectal prolapse are neurological and muscular conditions, rare genetic familial conditions and as a result of chronic straining with constipation. In the majority of cases however no specific factor can be identified. In all cases the pelvic support structures are weakened and this often becomes more apparent in the elderly patient. Patients that have rectal prolapse also often tend to spend time straining to pass a bowel motion for prolonged periods. This chronic straining tends to aggravate their prolapse problems.
Investigations
You generally might not need any investigations as the diagnosis is clinical. Sometimes you will be recommended a colonoscopy to rule out any bowel pathology and sometimes further tests like colonic transit study or mri defaecogram if you have symptoms of constipation
What Is The Difference Between Haemorrhoids And Rectal Prolapse?
Haemorrhoids may also be felt as a bulging that comes down on passing a bowel motion. This is due to the anal cushions protruding down and out at the anal verge. With rectal prolapse it is the lining or indeed the full thickness of the bowel wall that comes out through the anus. Although haemorrhoids can protrude out at the anal verge they are only from the anal margin whereas the rectal prolapse may protrude out a considerable distance.
Is Rectal Prolapse Related To Bowel Cancers?
Rectal prolapse does NOT cause cancer however some of the symptoms of rectal cancer may be similar. Also rectal cancers have been known to be present at the same time as a rectal prolapse and therefore thorough investigation should be undertaken.
What Are The Treatment Options For Rectal Prolapse?
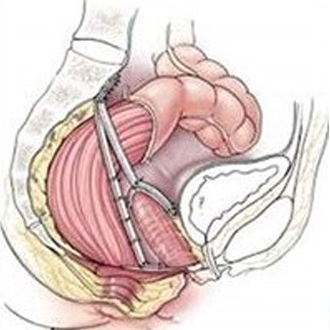
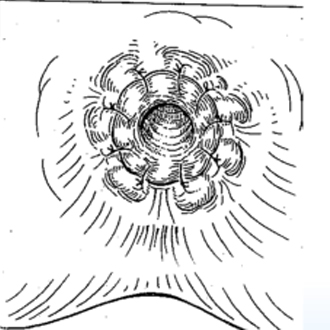
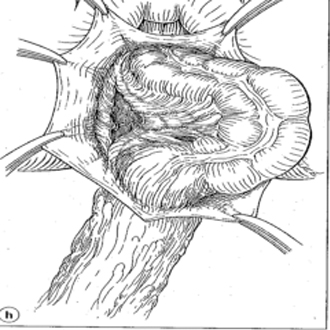
There are several treatment options for rectal prolapse. The one best suited to you will be decided by your surgeon. The surgery is termed a “rectopexy”. In general the surgery is aimed at either excising the prolapse or “hitching” the rectum back up inside to prevent it coming out. The surgery may involve operating on the anus alone (transanal approach) or approaching the prolapse from the abdominal side (transabdominal rectopexy). The choice of approach is determined by the surgeon.
What Is Involved In The Surgery Of Rectal Prolapse?
In the transanal approach the surgeon excises the prolapse from the lower end. In the abdominal approach the surgeon pulls the prolapse back into the abdomen and then secures it in order to prevent it falling back out. There are many different techniques used for securing the bowel in this way. In some cases the excess bowel may be removed and the ends then rejoined as part of the surgery. This surgery may now all be undertaken with a minimally invasive surgical approach (key-hole). The choice of surgery and approach used should be explained by the surgeon prior to the procedure.
What Can I Expect Immediately After My Surgery For Rectal Prolapse?
Patients often have some constipation initially after the operation. In cases where the surgery is performed in a “key-hole” fashion then the length of stay should only be a few days. In those that have had a section of their bowel removed then bowel function may be slow to return to normal. When the patient passes a bowel motion there may be some blood present however the palpable prolapse should be gone.
What Are The Chances Of The Rectal Prolapse Occurring Again?
Each of the surgical approaches has a reported incidence of recurrence. Those cases that are undertaken as a transabdominal approach have a recurrence rate of between 2 – 5% whereas the transanal approach has a much higher incidence of recurrence and is often reserved for patients with significant medical problems.