Diverticular Disease
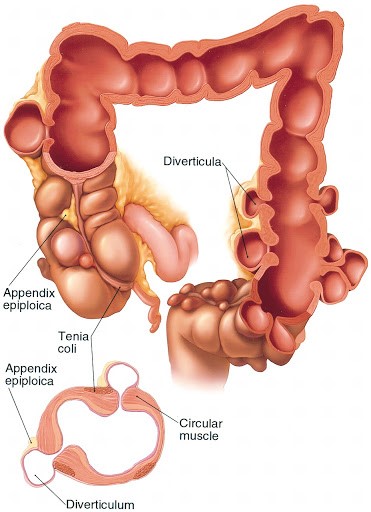
The development of small outpouchings or weakness of the bowel wall into small sac shaped bulgings is termed diverticulosis. Each one of these outpouchings or little blind-ended sacs from the bowel wall is termed a diverticulum. When a person has several of these outpouchings from their bowel wall then they are said to have diverticulosis. If one or more of these outpouchings become inflamed or infected then the person is said to have diverticulitis. The term diverticular disease is often used to describe both diverticulosis and diverticulitis.
How Did I Get Diverticulosis?
Diverticular disease is considered to be related to developing high pressure areas in the bowel and this pressure causing outpouchings of the wall itself. This is similar to a bulge on the bicycle tire from increased pressure. A lack of a high fibre diet over the years is thought to contribute to increased pressure in the bowel wall. With a lack of high fibre to make the bowel motion soft and bulky then high pressures are generated to move the stool on its way along the colon. This results in these diverticulae forming. By the age of 80 years well over half (50%) of the population are thought to have some evidence of diverticular disease due to their diet over the years. It is known however that diverticular disease may occur in much younger people also and can cause symptoms in those of the age of twenty and thirty upwards.
Is it a Cancer?
The simple answer is “NO” it is not type of cancer. There is no connection between diverticular disease and colorectal cancer. Diverticular disease itself is a non-cancerous condition and if you have diverticulosis then it will never turn into a bowel cancer. Some difficulty may arise as the symptoms of a bowel cancer and diverticular disease are often similar. It should also be remembered that a cancer may develop independently in someone that has already got diverticular disease. As the symptoms are often similar then investigation of the bowel to make sure that there is no cancer present is advisable.
What Are The Symptoms?
Patients with diverticular disease may have crampy pain usually on the left side, bloating, diarrhoea and a change in their bowel pattern. Occasionally there may be bleeding and this can be significant in a small number of patients. In those that develop diverticulitis then also symptoms of infection may occur. These include fever, chills and pain. There may be a change in their bowel habit either diarrhoea or constipation. The level of symptoms varies from patient to patient and depends upon the severity of the disease involved. In some patients further problems may occur which include perforation (leakage of the bowel), fistula formation (holes from the bowel to other organs such as the bladder) and abscess formation. These latter complications can be significant for the patient and require major surgery to correct.
How Are Patients Assessed For Diverticular Disease?
As the symptoms of colon cancer and diverticular disease may be similar then it is important to assess the colon to make sure there is nothing cancerous present. Usually patients undergo a colonoscopy to examine their bowel. This is a camera test that requires a short stay in the hospital. A CT scan (specialised x-ray) may also be used to examine for evidence of diverticulitis. In those that have more complex disease then other imaging investigations may be used but this is decided on an individual basis.
How Is Diverticular Disease Treated?
The vast majority of patients that have diverticulosis rarely need surgery. In those that have mild problems then the treatment is largely based on dietary measures. This may include increasing to a more high fibre diet, pain medication and other medications that will help relieve the symptoms. In those that have a mild attack of inflammation of the diverticulae (termed diverticulitis) then antibiotics are often required.
If a patient has more severe diverticulitis then the necessity of antibiotics and further treatment may necessitate that they are admitted to hospital for treatment. In the cases of abscess formation, fistula formation, perforation or significant bleeding then hospitalisation is usually required.
The treatment of these more complex cases is guided by the surgeon and may require surgery at some stage. Non surgical methods like CT guided drainage of abscess and antibiotics can be used in many cases and surgery avoided.
In patients who have sepsis or conservative management fail surgery is needed as condition can become life threatening. The surgery involved usually means taking away the section of the diseased bowel causing problems. This is a major colorectal operation and is indicated for those with complicated or recurrent diverticular disease problems.
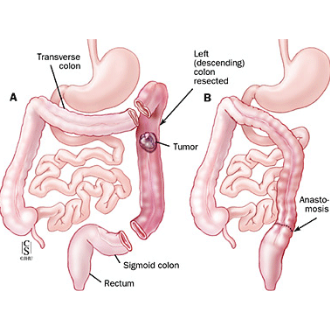
What Does The Surgery Involve?
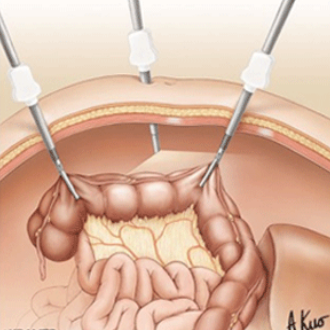
In those that need to have surgery for their diverticular disease then the surgeon will remove the section of the bowel causing problems. If suitable then the two ends of the bowel are joined back together. In some cases of more complex disease then it may be necessary to give the patient a temporary stoma or bag. This decision is based on the surgeon’s findings at the operation. The surgery may be carried out in a “key hole” (laparoscopic) or open manner depending upon the surgeon.
If diagnosed early and treated appropriately most patient would do well and majority will avoid surgery